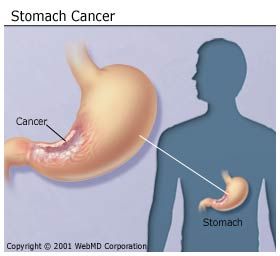
STOMACH CANCER
Stomach cancer, also called (GASTRIC CANCER) is a
malignant tumor arising from the lining of the stomach. There has been a
significant decrease in the number of people diagnosed with stomach
cancer in the past 60 years. According to the American Cancer Society,
the estimated numbers of new cases (people diagnosed with the condition)
and deaths from gastric cancer in the United States in 2012 will be:
- New cases: 21,320
- Deaths: 15,070
Stomach
cancers are classified according to the type of tissue where they
originate. The most common type of stomach cancer is adenocarcinoma,
which starts in the glandular tissue of the stomach and accounts for 90%
to 95% of all stomach cancers. Other forms of stomach cancer include
lymphomas, which involve the lymphatic system and sarcomas, which
involve the connective tissue (such as muscle, fat, or blood vessels).
Stomach cancer may often be cured if it is found and
treated at an early stage. Unfortunately, the outlook is poor if the
cancer is already at an advanced stage when discovered. In most cases,
stomach cancer is found at later stages.
What Causes Stomach Cancer?
The exact cause of stomach cancer is unknown, but a number of factors can increase the risk of the disease, including:
- Gender -- men have more than double the risk of getting stomach cancer than women.
- Race -- being African-American or Asian may increase your risk.
- Genetics -- genetic abnormalities and some inherited cancer syndromes may increase your risk
- Geography -- stomach cancer is more common in Japan, the former Soviet Union, and parts of Central America and South America.
- Blood type -- individuals with blood group A may be at increased risk.
- Advanced age -- stomach cancer occurs more often around ages 70 and 74 in men and women, respectively.
- Family history of gastric cancer can double or triple the risk of stomach cancer.
- Lifestyle factors such as smoking, drinking alcohol, and eating a diet low in fruits and vegetables or high in salted, smoked, or nitrate-preserved foods may increase your risk
- Helicobacter pylori (H. pylori) infection of the stomach. H. pylori is a bacterium that infects the lining of the stomach and causes chronic inflammation and ulcers.
- Certain health conditions including chronic gastritis, pernicious anemia, gastric polyps, intestinal metaplasia, and prior stomach surgery.
- Work-related exposure due to coal mining, nickel refining, and rubber and timber processing and asbestos exposure.
What Are the Symptoms of Stomach Cancer?
In the early stages of stomach cancer, you may have very few symptoms. These may include:
- Indigestion and stomach discomfort
- A bloated feeling after eating
- Mild nausea
- Loss of appetite
- Heartburn
These symptoms are similar to those caused by a
peptic ulcer. If you are experiencing any of these symptoms you should
see your health care provider so that a proper diagnosis can be made and
timely treatment given. A stomach cancer can grow very large before it
causes other symptoms.
In more advanced cancer, you may have:
- Discomfort in the upper or middle part of the abdomen.
- Blood in the stool (which appears as black, tarry stools).
- Vomiting or vomiting blood.
- Weight loss.
- Pain or bloating in the stomach after eating.
- Weakness or fatigue associated with mild anemia (a deficiency in red blood cells)
How Is Stomach Cancer Diagnosed?
Your health care provider can often detect advanced
stomach cancer by performing a physical exam. He or she may find
enlarged lymph nodes, an enlarged liver, increased fluid in the abdomen
(ascites), or abdominal lumps felt during a rectal exam.
However,
if you are having vague symptoms, such as indigestion, weight loss,
nausea, and loss of appetite, screening tests may be recommended. These
tests may include:
X-Ray Exams of the Digestive Tract
Colonoscopy is usually the preferred test used to
examine the digestive tract. However, there are several commonly
performed X-ray tests that allow your doctor to examine your digestive
tract from the esophagus to the rectum.
These
tests utilize barium or an iodine-containing agent that allows
visualization of the digestive tract and a form of X-ray machine called
fluoroscopy. Fluoroscopy allows part of the body to be studied in motion
and recorded on a video monitor.
The term inflammatory bowel disease
(IBD) describes a group of disorders in which the intestines become
inflamed. The likeliest cause is an immune reaction the body has against
its own intestinal tissue.
Two major types of IBD are ulcerative colitis and Crohn's disease.
Ulcerative colitis is limited to the colon or large intestine. Crohn's
disease, on the other hand, can involve any part of the gastrointestinal
tract from the mouth to the anus. Most commonly, though, it affects the
small intestine...
Fluoroscopic examinations of your GI tract may be
performed in a doctor's office, a commercial X-ray facility, or a
hospital. These tests are usually called either an "upper GI" or a
barium or contrast enema or a "lower GI", depending on the organs to be
studied.
Upper GI Tests
Upper GI tests use X-rays to examine the esophagus,
stomach, and first part of the small intestine (the duodenum). See the
article The Digestive System to learn more about these organs.
For these tests, you need to drink barium. As the
barium passes through the digestive tract, it fills and coats the
esophagus, stomach, and first part of the small intestine making them
more visible with X-ray. Then a fluroscope machine is held over the part
of the body being examined and transmits continuous images to a video
monitor.
This upper GI test is used to diagnose:
- Hiatal hernias
- Ulcers
- Tumors
- Esophageal varices
- Obstruction or narrowing of the upper GI tract
It may also be used to determine the cause of:
- Swallowing problems
- Reflux symptoms (dyspepsia or heartburn)
- Abdominal pain
- Diarrhea
- Unexplained vomiting, weight loss, or bleeding
There are several types of tests used to view the upper GI tract, including:
- Barium swallow. This is an X-ray test that examines how food moves down the esophagus to the stomach. Approximate time: 30 minutes.
- Modified barium swallow. This test looks at the beginning of swallowing from the mouth to the pharynx and down to the esophagus. Approximate time: 30 minutes to 1 hour.
- Upper GI series. This is an X-ray examination of the esophagus, stomach, and upper part of the small intestine. Approximate time: 30-45 minutes.
- Small bowel series. This is an X-ray examination of the small intestine (small bowel). Approximate time: 2 to 4 hours, depending upon how long it takes for the barium to reach the colon.
Lower GI Tests
Lower GI tests or barium enemas are used to examine
the large intestine and the rectum. For this test, barium or an
iodine-containing liquid is introduced gradually into the colon through a
tube inserted into the rectum. As the barium passes through the lower
intestines, it fills the colon, allowing the radiologist to see growths
or polyps and areas that are narrowed. The fluoroscope is held over the
part of the body being examined and transmits continuous images to the
video monitor.
This lower GI testing is used to detect:
- Colon polyps
- Tumors
- Diverticular disease
- Gastroenteritis
- Strictures or sites of narrowing and obstruction
- Ulcerative colitis or Crohn's disease
- Other causes of abdominal pain or blood, mucus, or pus in the stool
There are several types of tests used to view the lower GI, including:
- Air contrast barium enema (double contrast barium enema). This is an X-ray examination of the large intestine (colon). Barium and air are introduced gradually into the colon by a rectal tube. Approximate time: 1 hour.
- Barium enema. This is an X-ray examination of the large intestine (colon). Barium is introduced gradually into the colon by a rectal tube. Approximate time: 1 hour.
With the barium or contrast enema, the colon is
filled with a contrast material containing barium or iodine-containing
contrast (a liquid that lights up on X-ray) by running it through a tube
inserted into the rectum. The barium blocks X-rays; therefore the
colon, when filled with the agent, shows up clearly on the X-ray
picture.
The air contrast study is slightly different. The
colon is first filled with some barium, and then the colon is filled
with air. This technique provides a more detailed picture of the lining
of the colon, improving the procedure's ability to detect small polyps
or inflammation.
What Should I Do Before the Upper or Lower GI Studies?
Preparation for upper GI or lower GI testing usually
includes making dietary changes (such as following a low-fiber diet for
two to three days before the test), not smoking for 12 to 24 hours
before the test, not taking any medications for up to 24 hours before
the test and not eating anything for 12 hours before the test. Your
doctor will give you specific instructions. Never stop taking any
medications without first discussing it with your doctor.
Additional preparation for the lower GI test usually
includes taking oral laxatives and an enema the night before the test.
Please follow the pretest directions given to you by your doctor
carefully and ask questions if you do not understand them.
What Happens During the GI Tests
During GI testing:
- You will be positioned on a tilting X-ray table by the technologist. For an upper GI test, the table usually starts in a vertical position, with the person standing. For a lower GI test, the table usually starts in a horizontal position, with the person lying on his or her back or stomach. The table will be tilted at various angles during the test to help spread the barium solution throughout the body so that different views can be seen on the fluoroscope. During the test, the radiologist may put pressure on your abdomen to get a clearer image on the fluoroscope.
- Although the barium solution given in an upper GI test is unpleasant tasting, there is no pain and little discomfort during the procedure. The lower GI test may cause some discomfort, including cramps and a strong urge to have a bowel movement.
- After the barium enema is administered in a lower GI test and a few X-rays are taken, you will be helped to the bathroom (or given a bedpan) and asked to move your bowels to expel as much of the barium as possible. Then you will go back to the X-ray examination room where more X-rays will be taken of the barium solution that remains on the lining of the intestine. In some cases, air will be injected slowly into the colon (air contrast barium enema) to provide further contrast on the X-rays to detect abnormalities.
X-Ray Exams of the Digestive Tract
What Happens After the GI Tests?
Generally you can resume your usual activities and
normal diet immediately after your GI tests. But, drink plenty of fluids
(unless fluid is restricted for another medical condition), especially
if the test is an upper GI and/or small bowel series. The barium tends
to constipate people. Drinking 8-10 glasses of water or juice per day
for three days will help you to eliminate the barium from your colon.
It is normal for your stool to have a white or light color for up to three days after the test.
The barium enema given during the lower GI test may cause you to feel week or dizzy.
Are These GI Tests Safe?
There is virtually no risk with the upper and lower
GI tests, unless they are repeated several times within a few months'
time, when radiation exposure can become a risk. Although radiation
exposure is minimal, it is greater than for standard still X-rays. Steps
will be taken during the test to minimize radiation exposure.
Other risks include:
- Infection (very low risk with both the upper and lower GI tests)
- Tearing the intestinal wall during a lower GI test. Should this occur, surgery may be necessary. This is a very rare complication.
Who Should Not Receive GI Tests?
If you have an existing blockage or tear in the intestinal wall, the upper and lower GI tests should not be performed.
If you are pregnant or think you might be pregnant,
you should not have these tests unless absolutely medically necessary.
Talk to your doctor about other tests that can be more safely performed
to diagnose your problem during pregnancy.
When to Call Your Doctor After GI Tests
After the GI tests, call your doctor if you have:
- A temperature of 101 degrees Fahrenheit or higher. This could be a sign of infection and should be treated right away.
- A marked change in bowel habits (such as no bowel movement in two or three days after the test). Remember, it is normal for your stool to have a white or light color for up to three days after the test.
- Worsening of pain
- Any unusual rectal drainage
- Other symptoms that cause concern
- Questions about the test or the results.
I saw so many testimonies about Dr Itua a great HERBAL DOCTOR that can cure all kind of diseases and give you the rightful health to live a joyful life, i didn't believe it at first, but as the pain got worse and my life was at risk after visiting my therapist numeriuos times for combination of treatments. and no changes so i decided to take a try, I contacted him also and told him i want a cure for Vulvar cancer/ Testicular cancer and it was Stage IIIA, he gave me advice on what i must do and he delivered it to me in my state which i use according to his instruction, and today i must say I am so grateful to this man Dr Itua for curing me from Vulvar cancer/ Testicular cancer and for restoring me back to my normal health and a sound life,i am making this known to every one out there who have been living with cancers all his life or any sick person should not waist more time just contact him with his details below- WhatsApp- +2348149277967 Email drituaherbalcenter@gmail.com, believe me this man is a good man with Godly heart, this is the real secret we all have been searching for. Do not waste more time contact him today for you also to live a sound and happy life. he cure the following disease________Thyroid Cancer,Uterine cancer,Fibroid,Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Scoliosis,Brain Tumor,Fibromyalgia,Fluoroquinolone ToxicityBladder cancer,Brain cancer,Hiv,Herpes,Esophageal cancer,Gallbladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma
ReplyDeleteIntestinal cancer,Kidney cancer,Hpv,Lung cancer,Melanoma,Mesothelioma,Multiple myeloma,Neuroendocrine tumors
Non-Hodgkin lymphoma,Oral cancer,Ovarian cancer,Sinus cancer,Hepatitis A,B/C,Skin cancer,Soft tissue sarcoma,Spinal cancer,Stomach cancer,Vaginal cancer,Vulvar cancer,
Testicular cancer,Tach Diseases,Leukemia,Liver cancer,Throat cancer,
Syndrome Fibrodysplasia Ossificans ProgresSclerosis,Alzheimer's disease,Chronic Diarrhea,Copd,Parkinson,Als,Adrenocortical carcinoma Infectious mononucleosis.